SUPPLEMENTAL MATERIAL: End-of-life Care and Assisted Suicide
“The End,” an article in the September/October 2013 issue of the Humanist, tells a very personal account of one family’s experience with end-of-life care and death with dignity. Below, you’ll find more information on terminology, legality, and resources.
Rational Ends
 While the terms are often used interchangeably, “euthanasia” and “assisted suicide” aren’t synonymous. To understand the legal and ethical questions surrounding end-of-life decisions, one must first be able to distinguish the concepts being discussed:
While the terms are often used interchangeably, “euthanasia” and “assisted suicide” aren’t synonymous. To understand the legal and ethical questions surrounding end-of-life decisions, one must first be able to distinguish the concepts being discussed:
Euthanasia: Intentionally causing the death of a person with the intent of alleviating suffering or providing some other benefit to the deceased. Often used to describe voluntary euthanasia, wherein the dying person requests that they be killed. Non-voluntary euthanasia (also called mercy killing) describes a situation where the individual can’t provide explicit consent, for example when someone is comatose. Involuntary euthanasia is bringing a patient’s life to an end against their will.
Assisted Suicide: Helping a person end their life. The individual is required to take the final action but they receive assistance in creating the situation wherein they can do so (for example, acquiring supplies).
Physician-Assisted Suicide: When a medical doctor provides either instructions or the means for a patient to carry out suicide. The most famous example, of course, is Dr. Jack Kevorkian, pictured above.
Legality
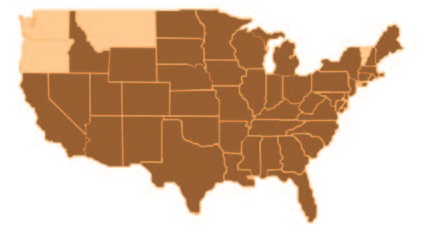
Euthanasia is legal in the Netherlands, Belgium, and Luxembourg; assisted suicide is legal in Switzerland. In the United States., individual states must determine whether to allow or outright ban assisted suicide. To date, four states provide a legal option for physician-assisted suicide only:
Oregon: The ballot measure of 1994 known as the “Death With Dignity Act” allows for a terminally ill patient to request a lethal dose of medications from a doctor, a request that a second physician must approve.
Washington: This state’s version of the “Death With Dignity Act” was approved by voters in 2008 with nearly 58% approval. Under the law, any Washington resident with a prognosis of six months or less to live can request lethal injection from a physician.
Montana: The 2009 court case Baxter v. Montana, as ruled by the state’s Supreme Court, allows physicians to use the argument of consent if they are charged with a crime for assisting in a patient’s suicide.
Vermont: In May the legislature passed the “End-of-Life Choices” law, a provision allowing patients who have been diagnosed by two doctors as having six months or less to live to request a doctor-assisted death.
Resources
 There are several groups in the United States that focus on end-of-life decisions:
There are several groups in the United States that focus on end-of-life decisions:
Compassion and Choices – The Hemlock Society merged with Compassion in Dying to form an advocacy non-profit that works legislatively to create new, legal options for patients who want to pursue assisted suicide.
Death With Dignity National Center – A national legal non-profit established to defend the Oregon Death With Dignity Law in the courts while also tracking and advocating for new assisted-suicide legislation around the country.
ERGO (Euthanasia Research and Guidance Organization) – Founded by the former head of the Hemlock Society, ERGO provides books, videos, and other media designed to help those considering assisted suicide to closely evaluate their options.
Final Exit Network – An all-volunteer organization that provides information to mentally competent persons on the peaceful ending of one’s life when one is suffering intolerably from an irreversible medical condition and one chooses to end one’s life. The organization also offers a compassionate presence at the time the person chooses to end his or her life.
Patients Rights Council -The PRC is focused primarily on educating the public on the options available to the dying, including euthanasia, advanced directives, pain control, and more.
